

Overview


Contact
What Is Meniscus Surgery?
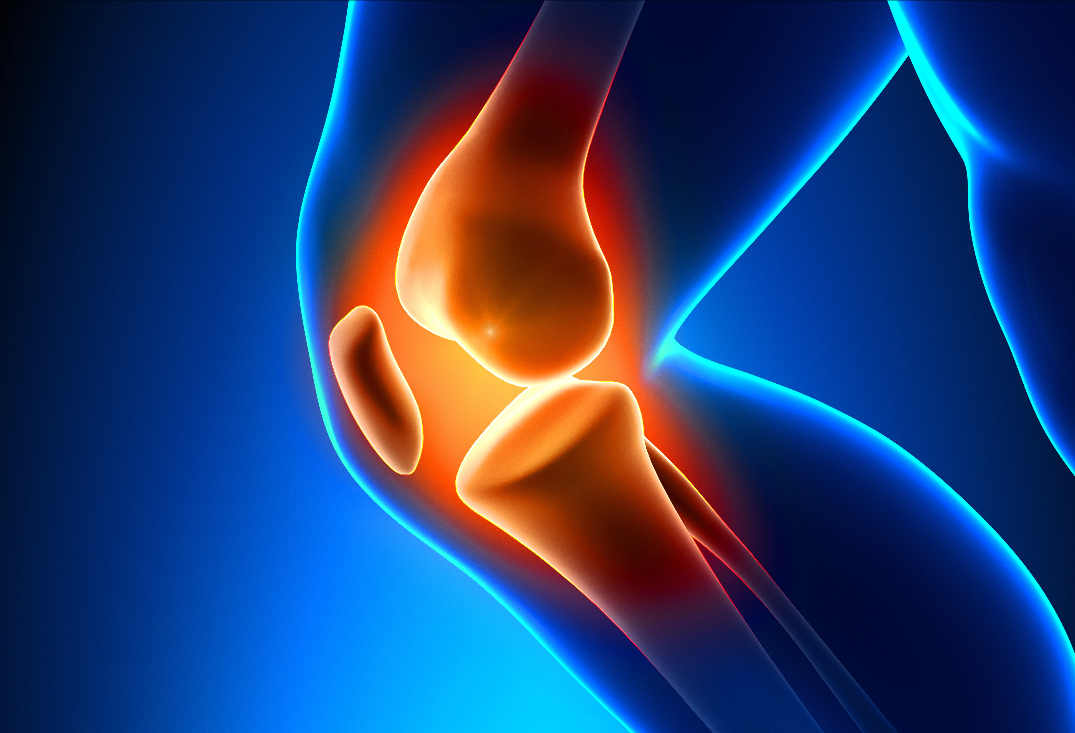
The knee menisci are two crescent-shaped fibrocartilaginous structures—the medial meniscus (C-shaped, attached to the medial collateral ligament and more prone to injury due to less mobility) and the lateral meniscus (O-shaped, more circular and mobile)—positioned between the femoral condyles and tibial plateau. They function as shock absorbers, distributing 50-70% of joint load, enhancing stability, aiding in lubrication and nutrition of articular cartilage, and limiting excessive motion during pivoting or twisting. The menisci have a peripheral vascular zone (red-red, outer third with blood supply from genicular arteries) that supports healing, a transitional red-white zone, and a central avascular white-white zone reliant on synovial diffusion. Collagen fibers are circumferentially oriented for hoop stress resistance, with radial ties for structural integrity.
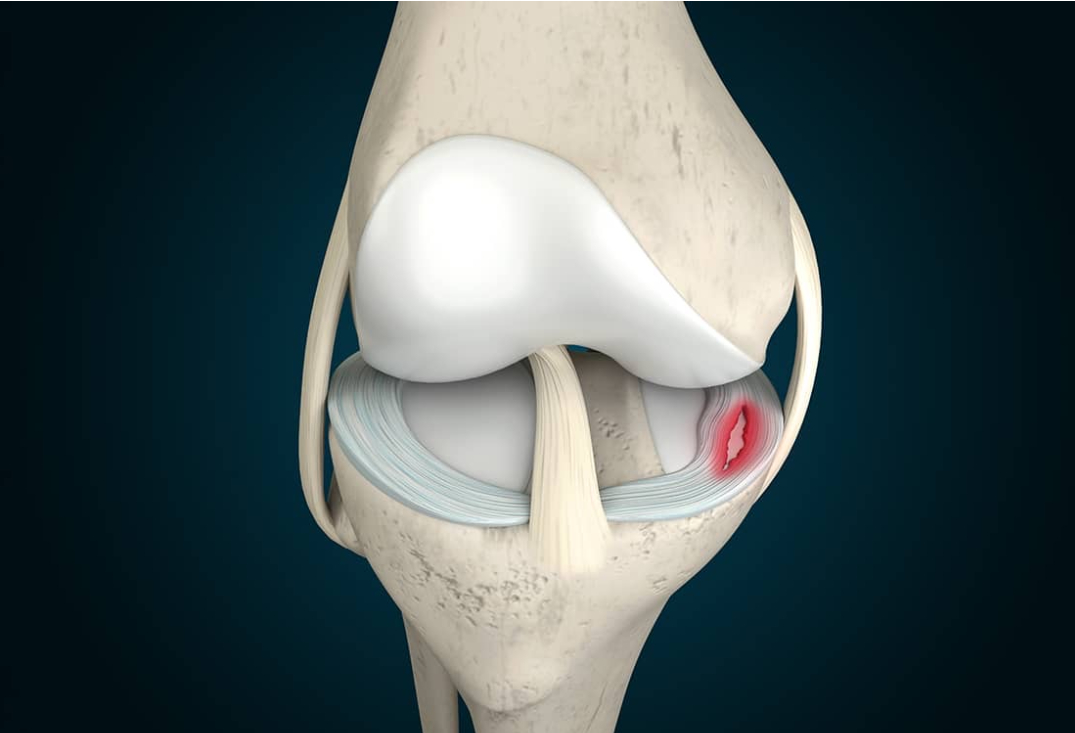
Meniscal tears arise from acute trauma (e.g., twisting during sports like soccer or skiing, often with ACL injury) or degenerative changes (e.g., in older adults from repetitive microtrauma), classified by pattern: vertical/longitudinal (stable or bucket-handle if displaced), horizontal (cleavage), radial (disrupting hoop stresses), oblique/flap, or complex (multiple planes). Tears in the avascular zone have poor healing potential, leading to symptoms like localized pain, swelling, mechanical locking/catching, joint effusion, and instability (e.g., giving way). Untreated tears accelerate articular cartilage wear, increasing osteoarthritis risk by 4-10 times due to altered biomechanics and load distribution. Clinical findings include joint line tenderness, positive McMurray or Apley tests, and MRI confirmation of tear morphology and location.
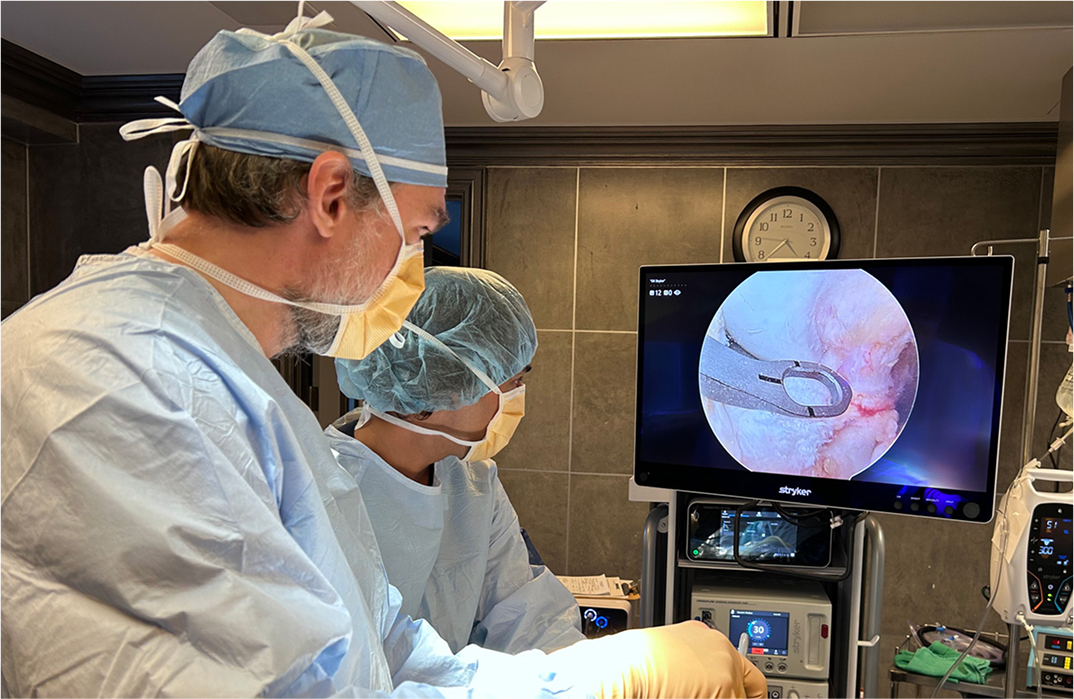
At OV Surgical, we elevate meniscus surgery in Canada with advanced arthroscopic techniques that minimize downtime and maximize results, often incorporating orthobiological augmentation with platelet-rich plasma (PRP). PRP is prepared from autologous blood centrifuged to concentrate platelets and growth factors (e.g., PDGF, TGF-β), injected intra-articularly or at the repair site to enhance inflammation modulation, cell proliferation, and tissue regeneration—particularly beneficial for repairs and transplants by improving vascularization and reducing re-tear rates by 20-30%. Through two to three tiny incisions (less than 1 cm), an arthroscope visualizes the joint, with fluid irrigation for clarity. The procedure typically lasts 15 minutes (partial meniscectomy) to 45 minutes (repair), depending on type, with meticulous debridement of unstable fragments and preservation of meniscal tissue to maintain function.
For irreparable tears in the avascular white-white zone or complex degenerative patterns, the damaged portion is selectively excised to create a stable rim. Using motorized shavers, biters, and punches, frayed edges are smoothed while preserving >50% of meniscal width to avoid increased contact stress (up to 100% in the medial compartment and 300% in the lateral compartment if total removal). PRP may be injected post-resection to reduce postoperative inflammation and promote residual tissue health.

For peripheral tears in the vascular red-red or red-white zones (e.g., vertical or bucket-handle), repair restores anatomy and function. Techniques include all-inside repair (using devices like Stryker Air or Arthrex FiberStitch) to place vertical mattress sutures without external knots), inside-out (sutures passed via cannulas and tied externally over capsule), or outside-in (needles passed percutaneously to retrieve sutures). The tear is reduced, and sutures spaced 3-5 mm apart; for bucket-handle tears, the displaced fragment is repositioned with graspers. PRP is applied directly to the repair site or via fibrin glue matrix to augment healing, stimulating fibroblast activity and collagen synthesis.
For young patients with prior total meniscectomy and symptomatic compartment overload, a size-matched cryopreserved allograft (medial or lateral meniscus with or without bone plugs) is transplanted. Via mini-arthrotomy or arthroscopic assistance, the native remnant is debrided to a stable rim, and the allograft is prepared with bone plugs or sutures. It is inserted through a portal, secured with transosseous sutures or anchors for the horns and peripheral capsule stitching. Alignment correction (e.g., osteotomy) may be concurrent. PRP augmentation involves soaking the allograft or injecting at fixation sites to enhance integration and vascular ingrowth, reducing graft failure by promoting early revascularization.
Recovery
Post-procedure, our evidence-based protocols integrate cryotherapy, neuromuscular electrical stimulation (NMES), and progressive physiotherapy to accelerate healing. Expect immediate weight-bearing as tolerated without crutches, with early range of motion (ROM) to full extension/flexion within days. Customized rehab plans aim for swelling control in week 1, quadriceps activation via straight-leg raises, and stationary biking by week 2. Strength milestones include closed-chain exercises (e.g., squats) by weeks 2-4, with most patients achieving sports clearance by 6 weeks, verified through quadriceps strength (>80% symmetry) and functional tests like single-leg hops. PRP augmentation may shorten by reducing effusion and inflammation.
For repairs, weight-bearing is protected (partial with crutches) for 4-6 weeks in a hinged brace locked at 0-90 degrees flexion to avoid shear forces. PROM begins day 1, progressing to active ROM by week 4. Rehab focuses on patellar mobilizations and isometrics initially, advancing to cycling (no resistance) at week 4 and resistance training (e.g., leg presses) by week 8. Full motion by 6-8 weeks, strength by 3 months, and sports in 4-6 months, assessed via stability exams and hop tests (>90% symmetry). PRP may be used with the goal of modulating inflammation and enhancing healing rates.
Mensicus allograft transplantation rehab is more cautious: non-weight-bearing for 4-6 weeks with a brace, emphasizing PROM to 90 degrees flexion initially. Gradual weight-bearing starts week 6, with closed-chain strengthening by week 8 and open-chain by week 12. Milestones include full ROM by 8-12 weeks, strength recovery by 4-6 months, and high-impact sports by 6-12 months. PRP augmentation promotes faster incorporation and may improve long-term viability. We emphasize psychological readiness for all, ensuring mental preparation for activity resumption


Benefits
With success rates of 90-95% for partial meniscectomy (symptom relief), 80-90% for repairs, and 70-85% for transplantation (pain reduction, graft survival), private meniscus surgery at OV Surgical restores knee stability, prevents re-injury and can delay the onset of osteoarthritis progression. We will work with you to get you back to sports and/or other aspects of life that are important to you. Our patients report enhanced knee function, confidence, and quality of life, backed by meticulous follow-up and data-driven protocols.
FAQ
Contact
