

Overview


Contact
What Is Hip Arthroscopy for FAIS?
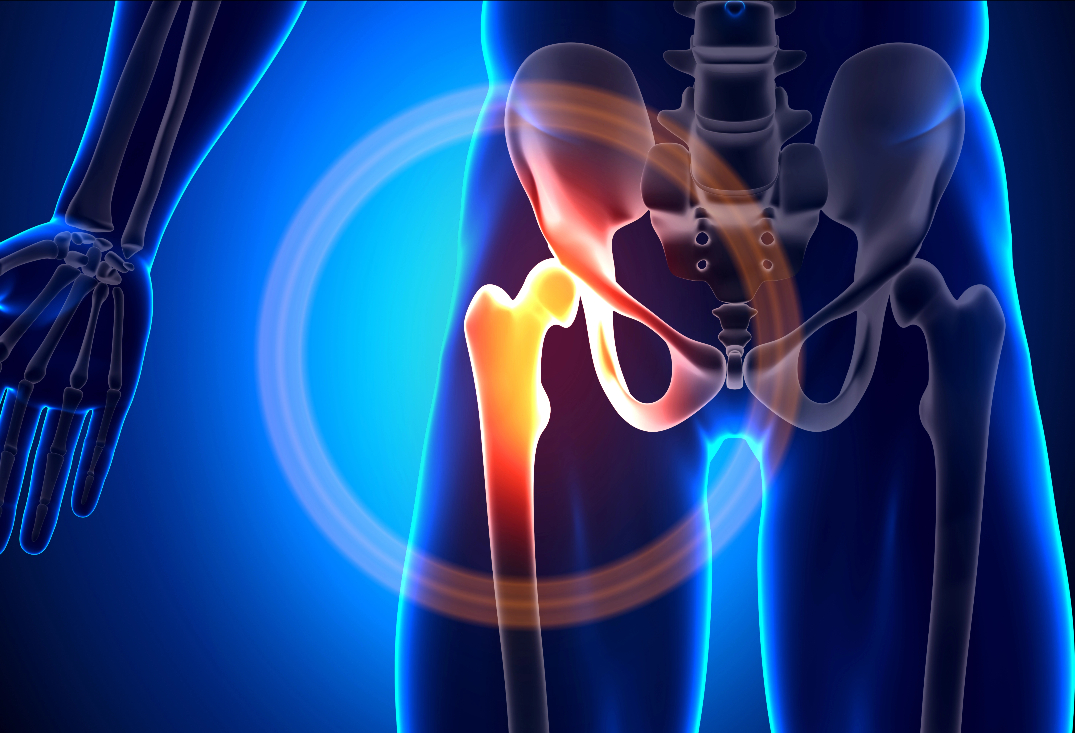
The hip joint is a ball-and-socket synovial joint where the spherical femoral head articulates with the deep acetabular socket of the pelvis, providing stability for weight-bearing while allowing multi-axial motion like flexion/extension, abduction/adduction, and internal/external rotation. Key structures include the acetabular labrum—a fibrocartilaginous rim that deepens the socket by 20-50%, enhances fluid seal for joint lubrication, and distributes load—and the articular cartilage covering both surfaces for low-friction gliding. The joint capsule, reinforced by ligaments (e.g., iliofemoral, pubofemoral, ischiofemoral), and surrounding muscles (e.g., gluteals, iliopsoas, adductors) maintain dynamic stability. The proximal femur features a neck connecting the head to the shaft, with the acetabular rim forming a horseshoe shape around the socket.
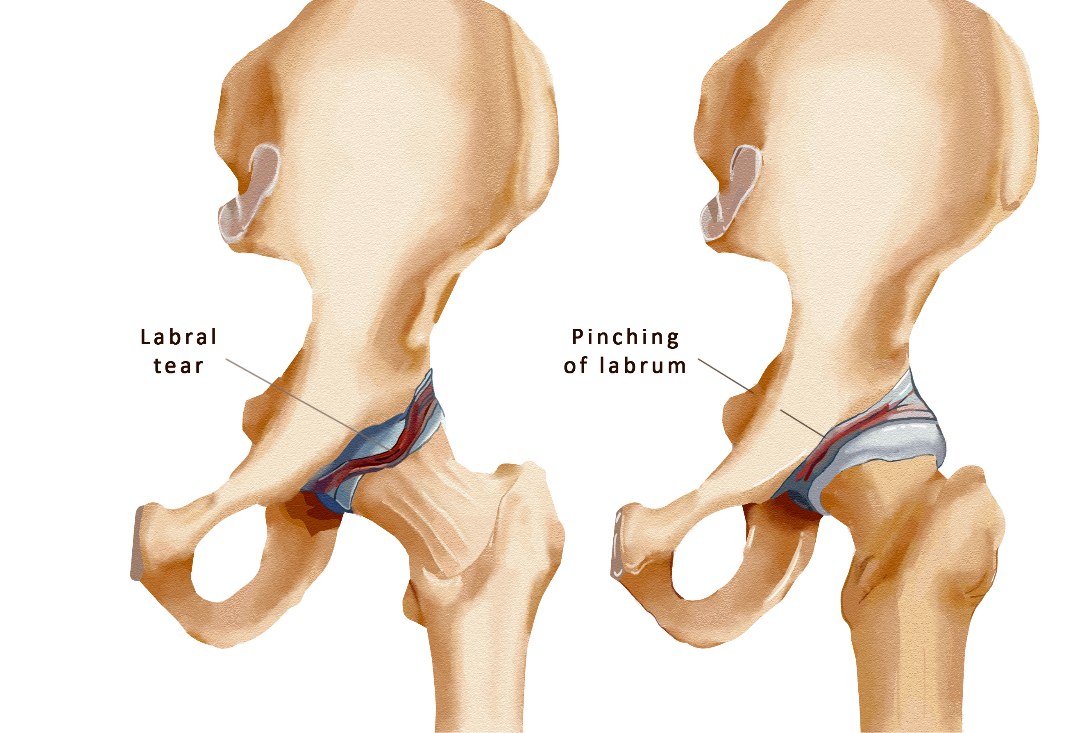
Femoroacetabular impingement syndrome (FAIS) arises from abnormal contact between the proximal femur and acetabular rim during hip motion, leading to pain and damage. It includes cam-type impingement (aspherical femoral head-neck junction causing pistoning into the acetabulum, often from bony bumps or pistol-grip deformity), pincer-type (overcoverage of the acetabulum from global or focal retroversion, protruding rim, or coxa profunda), or mixed (most common, 80%+ cases). Pathological changes include labral tears (fraying, detachment), cartilage delamination or defects (e.g., wave sign on acetabulum), and secondary issues like synovitis or loose bodies. Causes involve genetic factors, repetitive sports (e.g., soccer, hockey, ballet), or developmental anomalies like slipped capital femoral epiphysis. Symptoms feature groin pain worsened by flexion/adduction/internal rotation (positive FADIR test), stiffness, clicking, reduced range of motion, and positive impingement signs. Untreated FAIS can progress to labral degeneration, full-thickness cartilage loss, and early hip osteoarthritis.

At OV Surgical, we advance hip arthroscopy for FAIS and labral tears in Canada with minimally invasive arthroscopic techniques that minimize downtime and optimize results. Performed under general anesthesia with fluoroscopic guidance, the procedure uses two to three small incisions (less than 1 cm) around the hip—anterolateral, mid-anterior, and distal anterolateral portals—for portal placement under distraction (using a traction table to separate the joint by 8-10 mm). An arthroscope visualizes the central compartment (acetabulum, femoral head, labrum) and peripheral compartment (capsule, rim). Steps include capsulotomy for access, labral repair (reattaching torn labrum with suture anchors to restore the suction seal), acetabuloplasty (rim trimming with a burr to correct pincer deformity), and femoroplasty (reshaping the cam lesion by burring the femoral neck to restore sphericity, guided by fluoroscopy). Associated issues like cartilage repair or iliopsoas lengthening are addressed if needed. The capsule is repaired at closure for stability. The surgery lasts 1-2 hours, with focus on preserving neurovascular structures like the lateral femoral cutaneous nerve.
Recovery
Our evidence-based protocols use cryotherapy, neuromuscular electrical stimulation (NMES), and progressive physiotherapy, tailored to FAIS type and tissue repairs. In the protection phase (0-4 weeks), weight-bearing is partial (crutches for 2-4 weeks), focusing on pain control and gentle motion—stationary biking without resistance by day 2-3, passive range of motion (PROM) with circumduction, and isometric glute/quad activations to prevent adhesions. Precautions include avoiding extreme flexion/adduction/internal rotation and extension > 5-10 degrees.
From weeks 4-8 (active ROM and strengthening phase), full weight-bearing progresses, with active-assisted range of motion (AAROM) via hydrotherapy or ellipticals, and strengthening for hip abductors, extensors, and core (e.g., bridges, clamshells, 2-3 sets of 10-15 reps). Gait training normalizes patterns. By weeks 8-12 (functional strengthening phase), dynamic exercises like squats, lunges, and balance drills build endurance, with resistance bands for rotation and abduction. Advanced phases (12+ weeks) incorporate agility drills, plyometrics, and sport-specific training (e.g., cutting maneuvers for athletes). Full motion is typically achieved by 8-12 weeks, strength milestones by 3-4 months, and return to sports by 6 months, verified through tests like single-leg squat symmetry (>90%), hop tests, and hip outcome scores (e.g., iHOT-33). Psychological readiness addresses activity fears through gradual return-to-play protocols.


Benefits
With success rates of 80-90% in pain reduction and function improvement (e.g., 70-80% return to pre-injury sports levels), private hip arthroscopy for FAIS at OV Surgical alleviates impingement, preserves joint integrity, and delays osteoarthritis, supporting return to sports and daily life. Patients report enhanced function, confidence, and quality of life, backed by meticulous follow-up and data-driven protocols.
FAQs
Contact
