Overview


Contact
What Is Elbow UCL Reconstruction (Tommy John) or Internal Brace Repair?
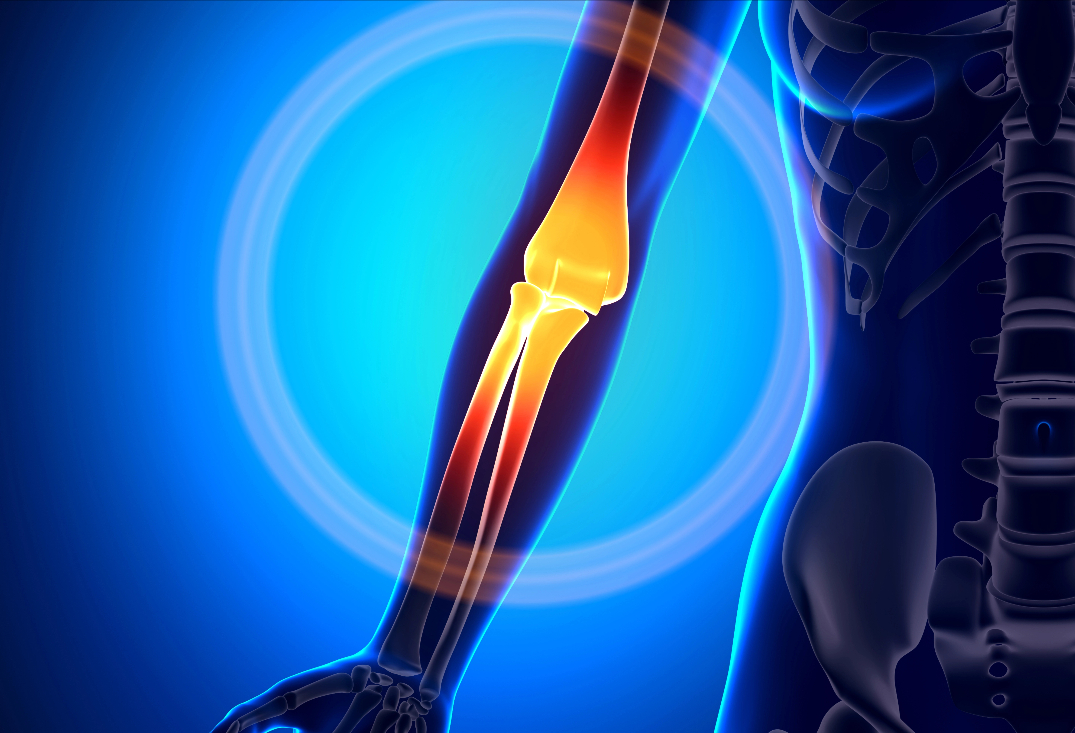
The elbow’s medial side features the ulnar collateral ligament (UCL), a three-bundle complex: anterior (primary valgus stabilizer from 20°-120° flexion), posterior (stability in full flexion), and transverse (minimal role). Originating from the medial epicondyle of the humerus and inserting on the sublime tubercle of the ulna, the anterior bundle resists valgus stress during overhead throwing. Surrounding structures include the flexor-pronator mass (dynamic support) and ulnar nerve (posterior to the ligament). The joint capsule and lateral ligaments provide additional stability for throwing motions generating up to 64 Nm of valgus torque.
UCL injuries typically occur from repetitive valgus overload in overhead athletes (e.g., baseball pitchers, javelin throwers), leading to microtears, attenuation, or acute rupture. Chronic stress causes anterior bundle thickening, calcification, or partial/full tears, often with associated flexor-pronator strains or ulnar neuritis. Acute avulsions may follow a single traumatic event. Symptoms include medial pain during acceleration phase, decreased velocity/control, tingling in the ring/little fingers (ulnar neuropathy), and positive valgus stress or moving valgus tests. Untreated, it progresses to chronic instability, secondary osteoarthritis, or inability to throw competitively.

At OV Surgical, we provide advanced elbow UCL procedures with tailored techniques—either UCL reconstruction with a graft, UCL repair with internal brace, or a hybrid of both—based on injury severity, minimizing downtime and optimizing results. Performed under general anesthesia with ulnar nerve monitoring, a muscle-splitting approach exposes the medial elbow via a 7-10 cm incision. Ulnar nerve transposition (submuscular or subcutaneous) is routine if symptomatic. The procedure lasts 60-90 minutes, with layered closure and splinting.
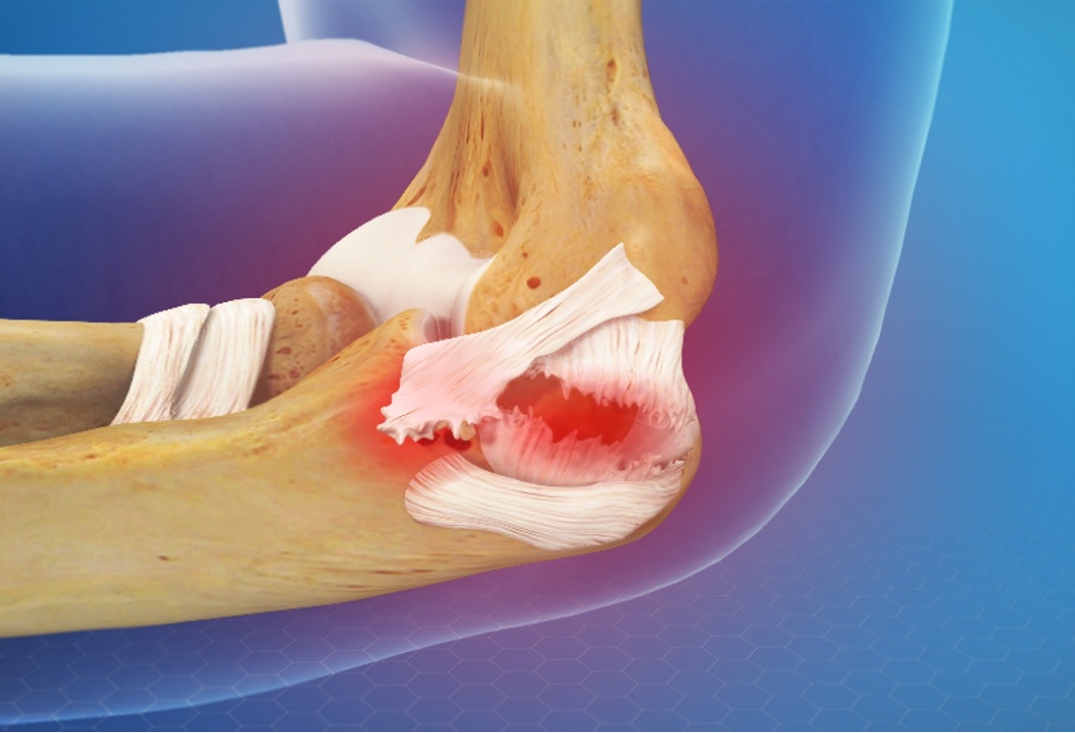
For complete or chronic tears unsuitable for repair, we use the bone tunnel technique. The native UCL is inspected; if irreparable, a graft (palmaris longus or gracilis autograft) is harvested and prepared. Bone tunnels are drilled in the medial epicondyle of the humerus and the sublime tubercle of the ulna. The graft is passed through these tunnels in a figure-of-eight configuration and secured with high strength sutures for robust fixation.
For acute or partial tears amenable to primary repair, we employ the Arthrex SwiveLock technique without reconstruction. The torn UCL is repaired using #0 FiberWire suture for direct approximation. Two 3.5 mm PEEK SwiveLock anchors, loaded with collagen-coated FiberTape suture, are placed at the ligament’s origin on the medial epicondyle and insertion on the sublime tubercle. The FiberTape spans the repaired ligament as an internal brace, tensioned appropriately and secured knotlessly to augment stability and promote healing. At the time of surgery, a primary repair of the UCL can also be performed for partial tears.
Recovery
Our evidence-based protocols use cryotherapy, neuromuscular electrical stimulation (NMES), and progressive physiotherapy, tailored to the procedure (reconstruction vs. repair with internal brace) and nerve involvement. In the protection phase (0-4 weeks), the elbow is braced at 90° with gradual ROM from 30°-100° by week 2, focusing on wrist/hand exercises and shoulder isometrics to prevent atrophy. Pain is managed with ice and medications.
From weeks 4-8 (active ROM phase), bracing allows full extension/flexion with active-assisted exercises, incorporating light pronation/supination and grip strengthening (2-3 sets of 10-15 reps). Valgus stress is avoided. By weeks 8-12 (strengthening phase), resistance progresses for forearm, wrist, and shoulder, with core/lower body conditioning. Advanced phases (12-24 weeks) include interval throwing programs starting at 18-24 weeks for reconstruction (or 8-12 weeks for internal brace repair), plyometrics, and sport-specific drills. Full throwing is cleared by 9-12 months for reconstruction (or 6-9 months for internal brace), verified through strength symmetry (>90%), valgus stress tests, and functional scoring (e.g., Kerlan-Jobe Orthopaedic Clinic score). Psychological readiness addresses return-to-sport anxiety through mental skills training.


Benefits
With success rates of 85-95% for reconstruction (recurrence <10%) and 90-95% for internal brace repair (faster return, recurrence <5%), private elbow UCL procedures at OV Surgical restore medial stability, prevent re-injury, and enable competitive throwing. Patients report enhanced function, confidence, and quality of life, backed by meticulous follow-up and data-driven protocols.
FAQ
Contact
