

Overview


Contact
What Is Knee Cartilage Restoration?
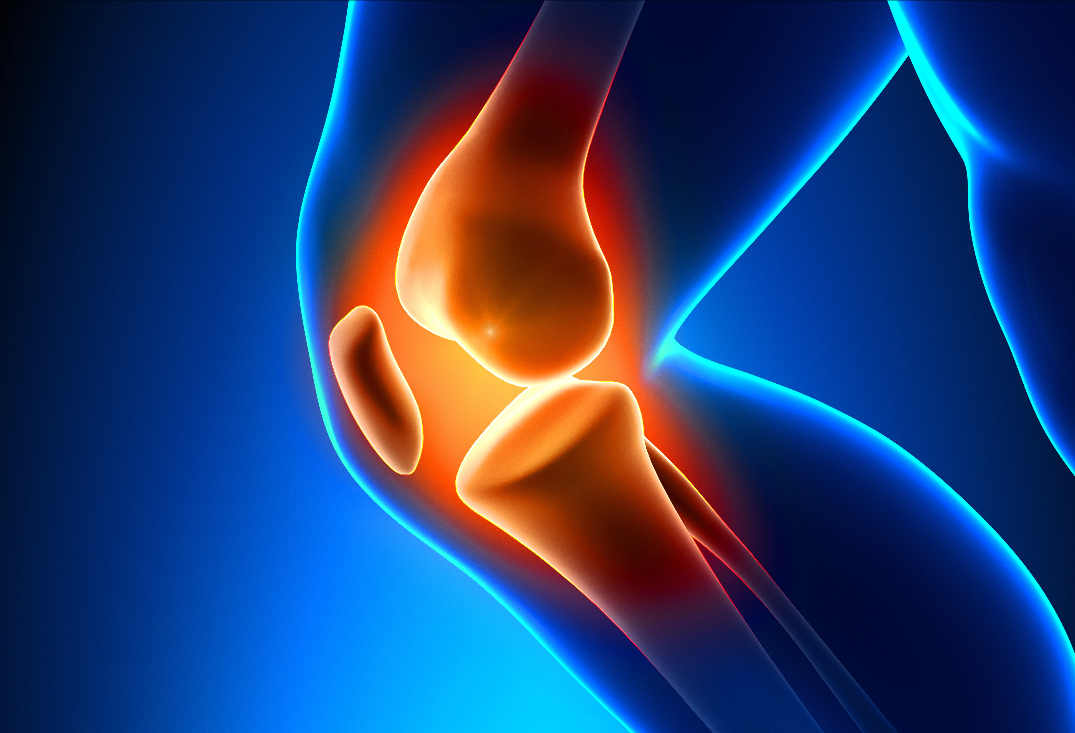
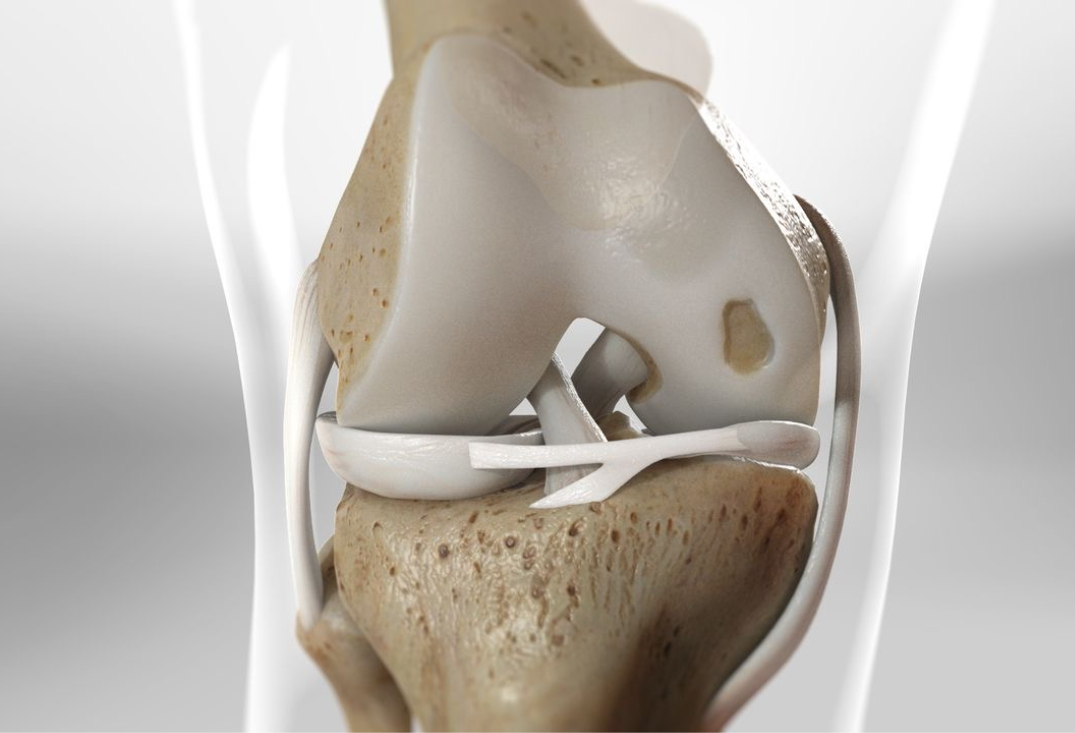
The knee’s articular cartilage is a smooth, resilient hyaline tissue (2-4 mm thick) covering the femoral condyles, tibial plateau, and patellar surfaces, enabling low-friction gliding, shock absorption, and load distribution during weight-bearing activities. Composed of chondrocytes embedded in an extracellular matrix of collagen (type II), proteoglycans, and water, it is avascular and aneural, relying on synovial fluid diffusion for nutrition. The subchondral bone beneath provides structural support, while zones include superficial (tangential fibers for shear resistance), middle (oblique for compression), and deep (radial for anchoring). Healthy cartilage withstands forces up to 5-10 times body weight, but its limited regenerative capacity makes restoration challenging.
Cartilage defects stem from acute trauma (e.g., impacts in sports like hockey or skiing), osteochondritis dissecans (OCD, avascular necrosis in adolescents), or degenerative conditions (e.g., early osteoarthritis from malalignment or meniscal loss). Cartilag defects are graded by the International Cartilage Repair Society (ICRS): grade I (superficial fissures), II (partial-thickness <50%), III (>50% but not to bone), IV (full-thickness to subchondral bone). Symptoms include pain, swelling, catching, and effusion, worsening with activity; untreated defects expand via edge loading, leading to subchondral cysts, bone edema, and progressive osteoarthritis. MRI or arthroscopy confirms size, depth, and associated issues like ligament instability and/or meniscus deficiency.

At OV Surgical, we elevate knee cartilage restoration in Canada with advanced, minimally invasive techniques that minimize downtime and maximize results, often incorporating orthobiological augmentation with platelet-rich plasma (PRP). PRP, derived from autologous blood centrifugation to concentrate platelets (4-5x baseline) and growth factors (e.g., VEGF, FGF), is injected or applied to stimulate chondrocyte proliferation, matrix synthesis, and anti-inflammatory effects—enhancing defect filling and integration by 20-40% across methods. Procedures are arthroscopic or mini-open, with defect preparation involving debridement to stable shoulders and subchondral drilling/microfracture to access marrow elements. Among the various surgical techniques that we use for cartilage repair, the most common approaches are outlined below. Decision making is based on activity level, size of the defect, involvement of subchondral bone, prior cartilage surgery, and associated pathology.
For full-thickness defects (ICRS III-IV, 2-10 cm²), AMIC combines microfracture with a collagen matrix scaffold. The defect is debrided to a contained lesion, and multiple 1-2 mm holes are drilled 3-4 mm apart into subchondral bone to release marrow-derived mesenchymal stem cells (MSCs) and clot formation. A bioresorbable collagen I/III membrane (e.g., Chondro-Gide) is cut to size, hydrated, and sutured or glued over the defect to stabilize the superclot and guide fibrocartilage formation. PRP is infiltrated beneath the matrix or mixed with the clot to boost MSC differentiation and hyaline-like tissue quality.
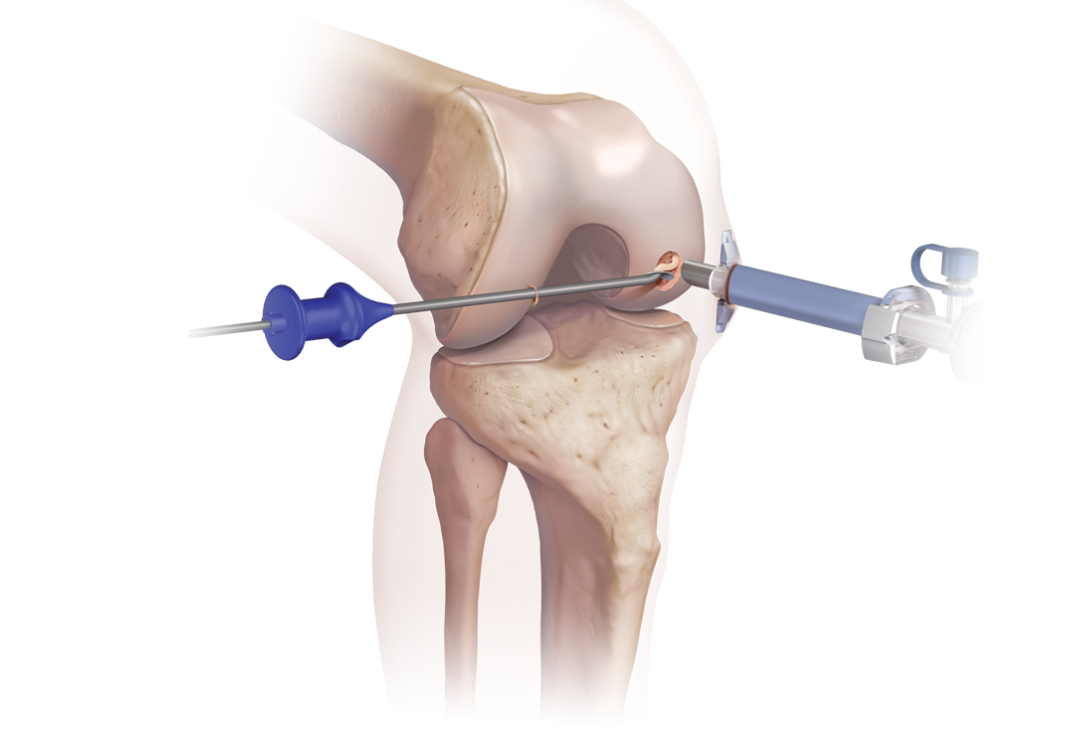
Ideal for contained defects (1-4 cm²), BioCartilage uses micronized allogeneic cartilage extracellular matrix (dehydrated, sterile) mixed with PRP to create a paste. The lesion is prepared with vertical walls and microfracture for bleeding base. The BioCartilage-PRP mixture (1:1 ratio) is applied to fill the defect flush with surrounding cartilage, covered by a fibrin glue seal or membrane for containment. This scaffolds MSC recruitment, promoting hyaline-fibrocartilage hybrid repair with better integration than microfracture alone; PRP augments by providing autologous growth factors for enhanced chondrogenesis and reduced apoptosis.

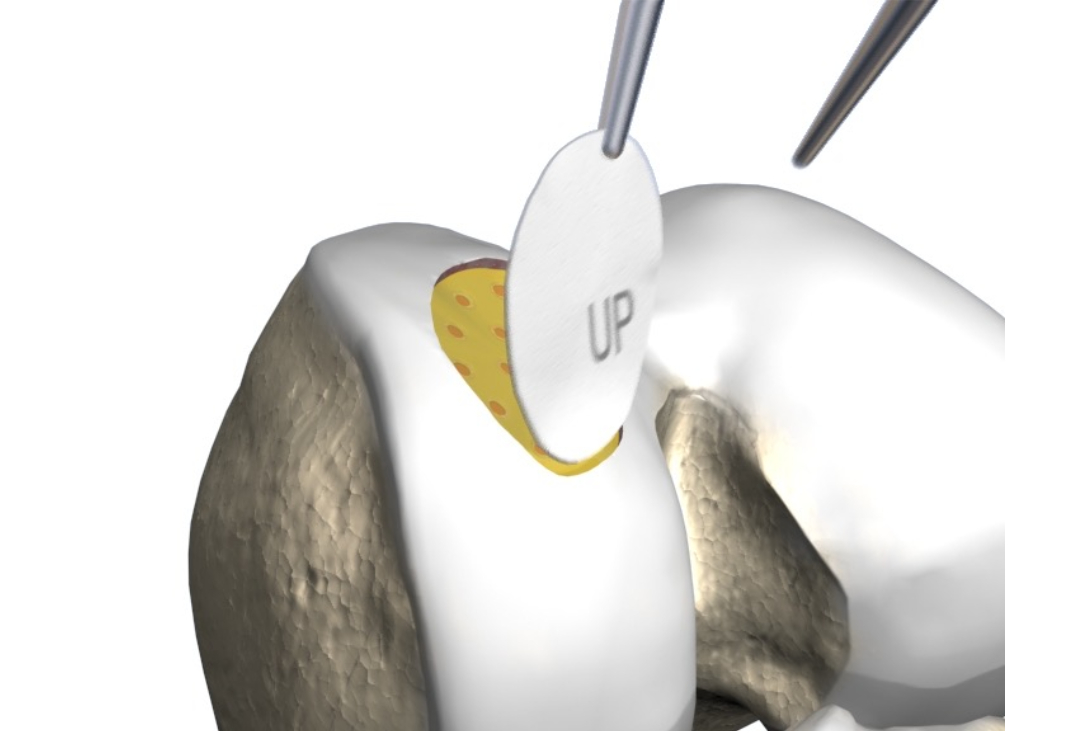
For defects <3 cm² with involvement of subchondral bone and/or after prior surgery, OATS harvests cylindrical plugs (6-10 mm diameter) from non-weight-bearing autologous sites (e.g., lateral femoral condyle or trochlea) using tubular chisels. The recipient defect is cored to matching depth, and plugs are press-fit in a mosaic pattern for congruent surface restoration with viable hyaline cartilage and bone. PRP is injected around plugs to improve osseous integration and reduce donor-site morbidity. OATS is a great procedure for small to medium defects in patients who want to return to sport quickly (~6 months).

For larger defects (>3 cm² or failed prior repairs), fresh osteochondral allografts (size-matched from donors) provide hyaline cartilage and subchondral bone. Via mini-arthrotomy, the defect is templated and reamed; the allograft is cut to fit (e.g., cylindrical or shell) and press-fit or fixed with screws/pins. Viability is maintained via hypothermic storage; PRP soaking or injection at interfaces enhances chondrocyte survival (up to 80-90%) and bony union, mitigating immune response and improving long-term graft incorporation.
Recovery
Post-procedure, our evidence-based protocols integrate cryotherapy, neuromuscular electrical stimulation (NMES), and progressive physiotherapy to accelerate healing and restore function, tailored to defect size (small <2 cm² vs. larger) and location (weight-bearing vs. non weigth-bearing). In the immediate protection phase (0-6/8 weeks), patients are non-weight-bearing with crutches and a hinged brace locked in extension to limit shear on the repair site, while allowing passive range of motion (PROM) exercises under therapist guidance to prevent adhesions—starting with continuous passive motion (CPM) machine from 0-60 degrees flexion, progressing to 90 degrees by week 2, alongside patellar mobilizations and heel slides. Pain management includes ice, elevation, and anti-inflammatories to control swelling and effusion.
From weeks 6/8-12 (active-assisted phase), crutches are weaned to partial weight-bearing (toe-touch to 50% body weight) and then full weight bearing by week 8. Active-assisted range of motion (AAROM) progresses with stationary biking (no resistance) or aquatic therapy, progressing to full passive ROM while avoiding deep squats or impact to protect cartilage integration. Submaximal isometrics for quadriceps, hamstrings, and hip stabilizers are introduced to rebuild neuromuscular control and prevent muscle atrophy. By weeks 12-16 (active strengthening phase), full weight-bearing continues to be targeted, with resistance exercises like closed-chain leg presses, mini-squats, and step-ups using body weight or light bands, emphasizing eccentric control to mimic functional loading. Advanced phases (16+ weeks) incorporate proprioceptive drills on balance boards, agility ladders, plyometrics (e.g., double-leg hops progressing to single-leg), and sport-specific simulations (e.g., cutting drills for athletes). Most patients achieve full motion by 8-12 weeks and strength milestones by 4-6 months, with clearance for high-impact sports in 6-12 months, verified through tests like knee strength assessments (>90% symmetry), single-leg hop distances, timed agility runs, and clinical exams (e.g., no effusion, stable gait). We emphasize psychological readiness, addressing fear of re-injury through gradual exposure and confidence-building exercises.


Benefits
With success rates of 75-85% for AMIC/BioCartilage/OATS, and 70-80% for allografts (for larger and more complex defects), private knee cartilage restoration at OV Surgical halts defect progression, delays osteoarthritis, and allows you to get back to sports and/or other aspects of life that are important to you. Our patients report enhanced knee function, confidence, and quality of life, backed by meticulous follow-up and data-driven protocols.
FAQ
Contact
